The Health Research Council (HRC), Te Aho o Te Kahu, the Cancer Control Agency, and the Ministry of Health have today announced $6.2 million in funding for research aimed at addressing the stark inequities in cancer care and survival for Māori and Pacific peoples in New Zealand.
HRC Chief Executive Professor Sunny Collings says a major focus of this new equitable cancer outcomes research funding is lung cancer, which is a leading cause of death and health inequity in New Zealand and has been highlighted as a priority area in the New Zealand Cancer Action Plan1.
“Māori are four times more likely to die from lung cancer than non-Māori, an unacceptable disparity that has remained unchanged for at least the past 20 years. If we are to eliminate the signifcant health inequities in cancer outcomes that exist in Aotearoa New Zealand and ensure that future public health initatives don’t unintentionally exacerbate them, it is vital that we conduct equity-focused research from the get-go,” says Professor Collings.
Professor Diana Sarfati, Chief Executive of Te Aho o Te Kahu, says the research themes were selected to align with the organisation’s commitment to improve equity in cancer outcomes in Aotearoa.
“We are prioritising lung cancer research because lung cancer is our biggest cancer killer - over 1700 people die of lung cancer each year - and our most inequitable cancer. We are excited to enable research that has the potential to make a massive difference for whānau living with lung cancer in Aotearoa.”
Māori epidemiologist Associate Professor Jason Gurney (Ngāpuhi) of the University of Otago, Wellington, and his team have received funding to draw together new and existing information to help improve lung cancer services for Māori in New Zealand, with a view to achieving equity in lung cancer survival for Māori by 2030.
“At 300 deaths per year, about the same number of Māori die from lung cancer as die from the six next most common causes of cancer death combined. Our own recent research shows strong survival disparities across all stages of lung cancer, suggesting that access to potentially curative treatment is not equal between Māori and non-Māori regardless of the stage,” says Associate Professor Gurney.
“This project will explicitly focus on understanding the role of cancer services in perpetuating inequities in lung cancer survival and identifying those factors that might be able to be modified in the short to medium-term.”
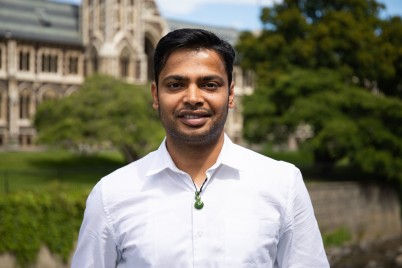
Also focused on achieving equity in lung cancer outcomes is University of Otago Associate Professor Aniruddha Chatterjee (pictured) and his team who have received $1.2 million in funding to develop an innovative, highly sensitive and cost-effective blood-based molecular test to identify lung cancers in New Zealand’s diverse population at an earlier stage.
“Although surgery and radiotherapy are effective treatments for early-stage lung cancer, 80 percent of patients are diagnosed with late-stage disease, when their tumours are no longer curative,” says Associate Professor Chatterjee.
“By developing a test that identifies the presence of tumours from plasma-dervied DNA, our team aims to improve the diagnostic performance and accuracy of the proposed low-dose computed tomography (CT) national lung cancer screening programme and improve lung cancer outcomes. Because this test would only require a peripheral blood sample, sampling could be carried out within the community by rural nurses, marae-based clinics and general practices at any time, reducing geographic and ethnic inequities.”
In addition to lung cancer, Dr Georgina McPherson from Waitematā District Health Board has received funding to identify potential contributors to the delayed diagnosis of endometrial or uterine cancer, which is on the rise in New Zealand, particularly among young pre-menopausal Pacific women. While Maria Ngawati (Ngāti Hine) from Māori public health provider Hāpai te Hauora Tapui will pilot a new model of cancer care service for Māori that involves oncology services and whānau ora providers partnering together to localise cancer care within Māori community settings.
Ministry of Health Chief Science Advisor Ian Town says the research projects will promote equitable healthy futures for all New Zealanders.
“We want to support all New Zealanders to live longer and have the best possible quality of life, and are focused particularly on Māori, Pacific, disabled and rural communities. This is also a major priority of the health and disability sector reforms. Research such as this will help inform how clinical care will be planned and delivered to meet the needs of all people who use the health system,” he says.
See below for the full list of recipients of the 2021 Equitable Cancer Outcomes Request for Proposals.
1 https://www.health.govt.nz/publication/new-zealand-cancer-action-plan-2019-2029
2021 Equitable Cancer Outcomes Request for Proposals - recipients
Funding stream 1: Lung Cancer Screening
(Funded by the Health Research Council and Te Aho o Te Kahu, the Cancer Control Agency)
- Professor Sue Crengle, Waitematā District Health Board
Lung cancer screening: Testing ethnicity weighting for risk prediction in Māori
36 months, $1,936,535
Funding stream 2: Improving Clinical Cancer Care
(Funded by the Health Research Council and the Ministry of Health)
- Associate Professor Aniruddha Chatterjee, University of Otago
A nationwide strategy to improve lung cancer outcomes with molecular testing
36 months, $1,222,392
- Associate Professor Jason Gurney, University of Otago, Wellington
Equity by 2030: Achieving equity in lung cancer survival for Māori
24 months, $799,945
- Professor Ross Lawrenson, Waikato District Health Board
Improving management and outcomes for patients with lung cancer
24 months, $719,825
- Dr Georgina McPherson, Waitematā District Health Board
Māori and Pacific women’s pre-diagnostic experiences of uterine cancer
12 months, $261,413
- Ms Maria Ngawati, Hāpai te Hauora Tapui
Te Pae Ora – Whānau ora navigation in local delivery of oncology care
36 months, $1,256,425